If you have kept up with us in the past year, you may have seen silicone suturing pads, partial-task trainers, and the plethora of other innovative applications for health science simulation at UCSF that can be made cost-effectively using 3D printing and other emerging technologies right here in the Library.
In the Makers Lab, we are excited to continue our exploration into this area of innovation to support the development of ideas that arise from our community of UCSF staff, faculty, students and researchers. A recent project we have been thrilled to support is the development of pelvis models for bone marrow biopsy training in the UCSF Division of Hematology and Oncology.
The UCSF Division of Hematology and Oncology offers the Hematology-Oncology Fellowship Training Program annually. The fellowship, devoted to training physician leaders in academic hematology and oncology, welcomes seven new fellows each year. Mari Collings, education manager within the UCSF Hematology/Oncology Education office, reached out to the Makers Lab early in May to organize a bone marrow biopsy simulation session for graduating fellows.
The bone marrow biopsy procedure involves the use of a manual drill to pierce through skin, tissue and muscle into the bone of the iliac crest of the pelvis. The drill punctures through a portion of the bone, and once it is far enough down a syringe is used to extract the patient’s bone marrow for sampling. There is little room for error when drilling into this area because the needle can puncture muscle, creating bruising and hematomas that can cause extreme discomfort and pain for the patient. Only local anesthetic is applied during the procedure and not much can be done to ease the pain of a hematoma once it occurs. To increase the likelihood of success for the procedure and to reduce patient discomfort and pain, rigorous training is therefore crucial.
Traditional bone marrow biopsy simulators are not only expensive, but are often unable to provide important tactile information for trainees, such as gauging depth and resistance for actual drilling or verifying the angle of entry for the needle. Locating the posterior superior iliac spine (PSIS) relies on physical palpation in particular.
The Makers Lab worked together with Dr. Gerald Hsu, Hematology/Oncology Fellowship Program director, Dr. Sam Brondfield, Hematology/Oncology fellow, and Dr. Derek Harmon, Anatomy Learning Center director, to devise a customizable and cost-effective solution that would address the issues with current simulator models.
After a few initial brainstorming sessions, the team decided on the key features for the simulation model, which consisted of four main components:
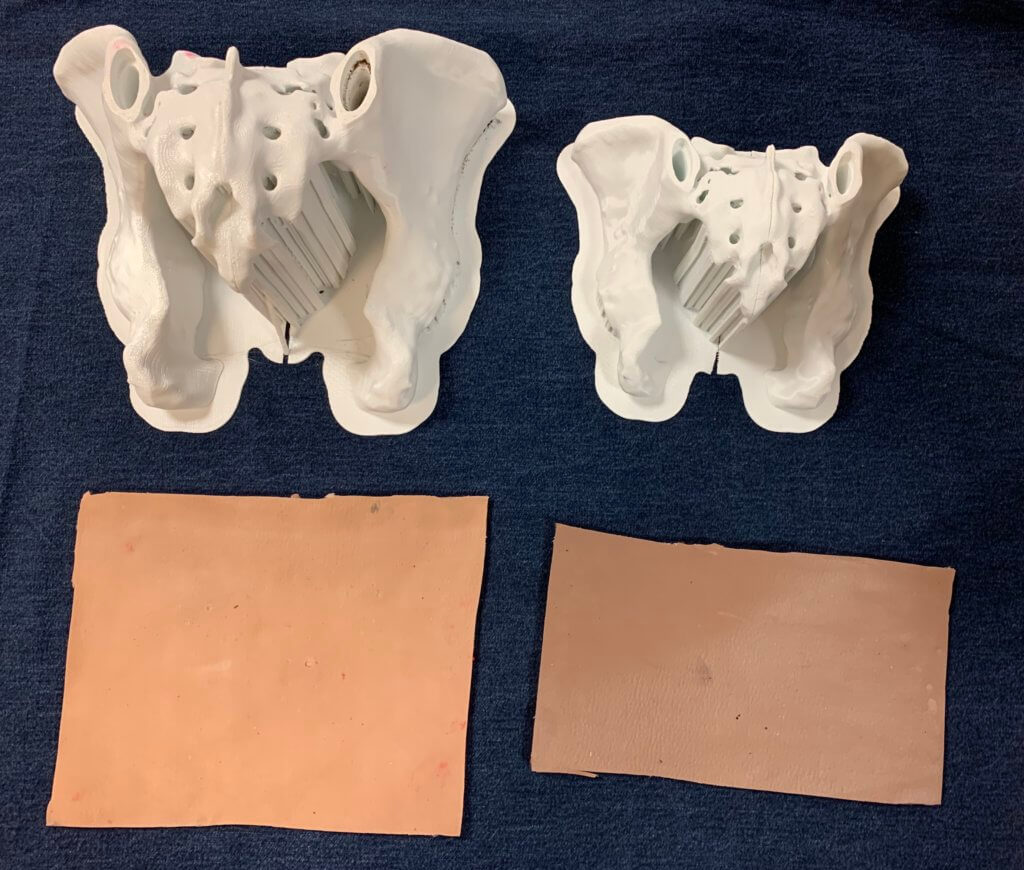
- 3D printed pelvis models with replaceable caps: 3D models of an adult male pelvis — acquired from the NIH 3D Print Exchange, a health science 3D model repository — printed at full scale and at 75-percent scale (to mimic a child-sized pelvis). The replaceable caps would be designed separately.
- Cork inserts: Pieces of cork would be inserted into the caps to simulate the resistance a hematologist would feel after piercing through the layer of bone, but before accessing the marrow. Drs. Hsu and Brondfield were interested in replicating the feeling of using a corkscrew to open a wine bottle.
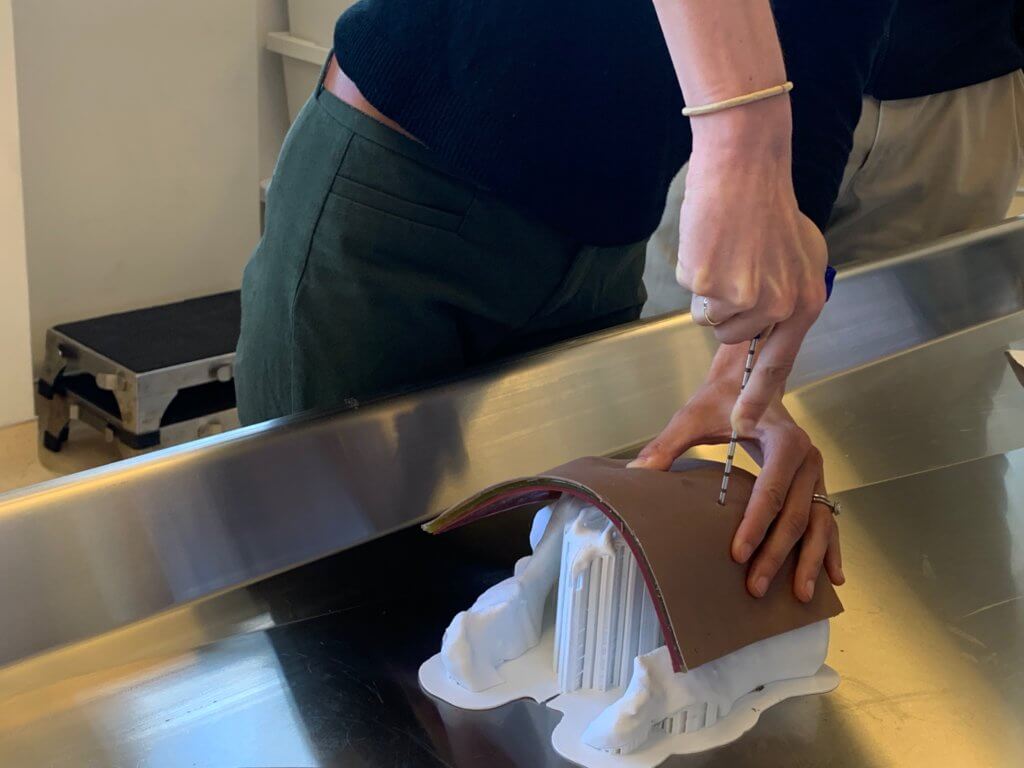
- Silicone suture pads: To make the model even more robust, silicone skin pads mimicking the fat, tissue, and muscle layers are draped on top of the pelvis model to assist fellows in realistically simulating the palpation process.
- Imitation bone marrow: A mixture of sand and water would fill the channel underneath the 3D printed pelvis caps to simulate the gritty texture of actual bone marrow.
While 3D printing pelvis models for each of the fellows was not impossible, it was definitely time-consuming considering the project’s timeline. Producing replaceable caps instead of pelvises ensured that each fellow would be able to have their own cap to drill through while optimizing for time and material. The pelvis itself would be reusable, and the caps would be able to be swapped out once they were drilled through.
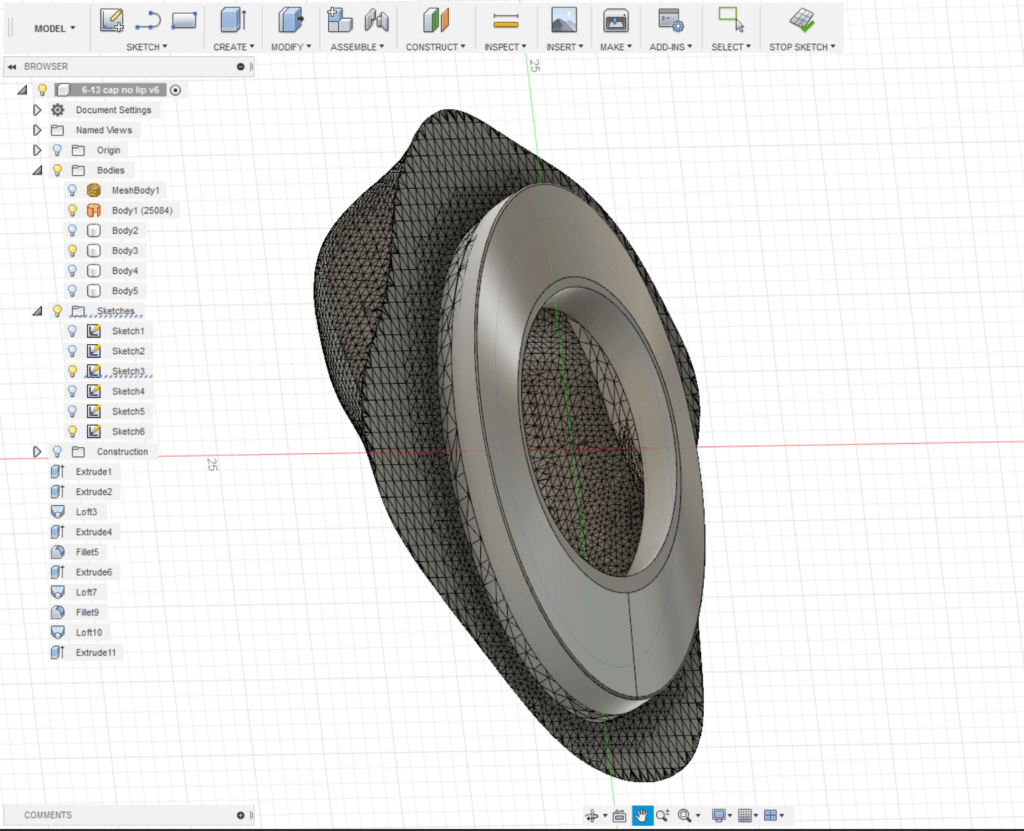

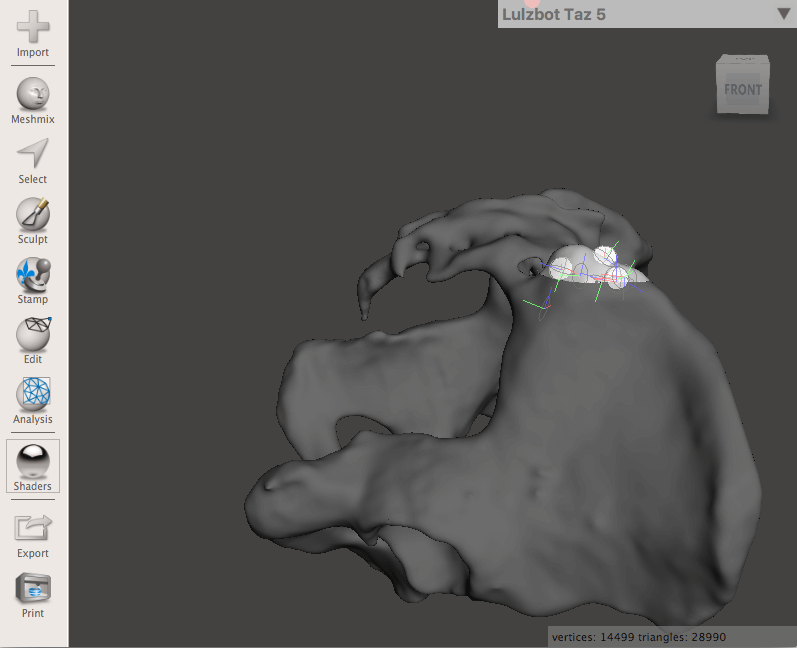
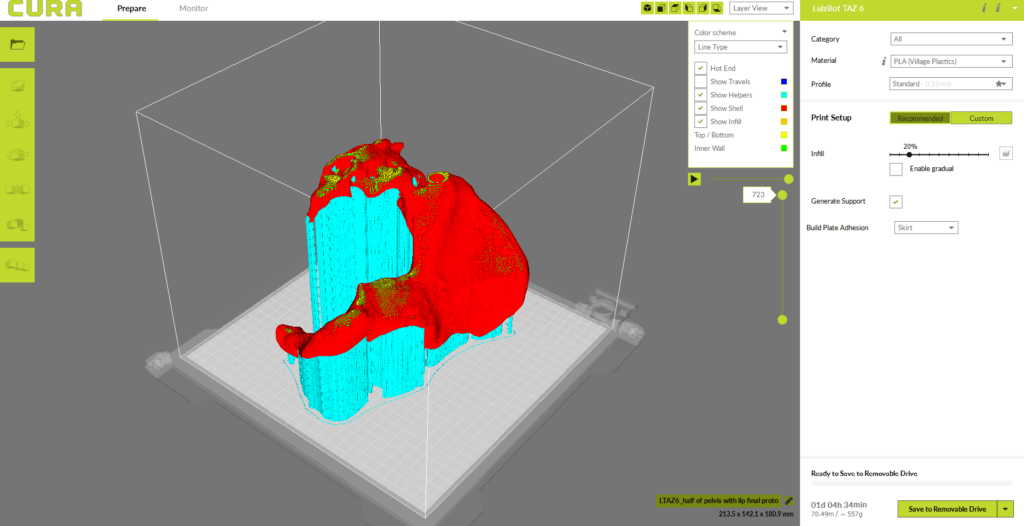
The pelvis cap and channel for inserting the bone marrow was modeled primarily using Meshmixer, an open-source 3D mesh software. The precise measurements of the cap’s “lip” was finalized using CAD design software Fusion 360 to ensure fit and prevent slipping during the simulation. Initial prototypes of the caps were 3D printed using a rigid liquid resin on the Form 2 SLA printer, but after conducting trials the texture and durability of PLA plastic was found to be most similar to that of bone. The final prototypes of the pelvis and caps were printed using the LulzBot TAZ 6 and Ultimaker 3 printers, respectively.
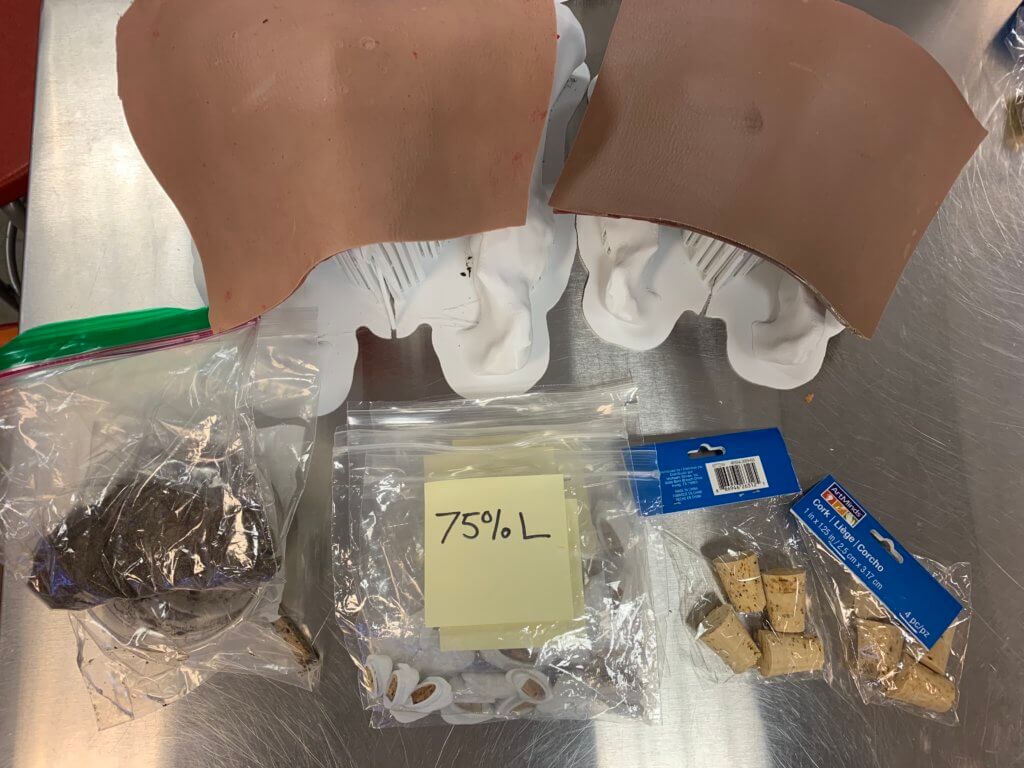
We were able to 3D print and deliver a total of forty pelvis caps along with two scaled pelvis models to the Anatomy Learning Center on the day of the simulation. The simulation demo itself was held in the center’s cadaver lab:

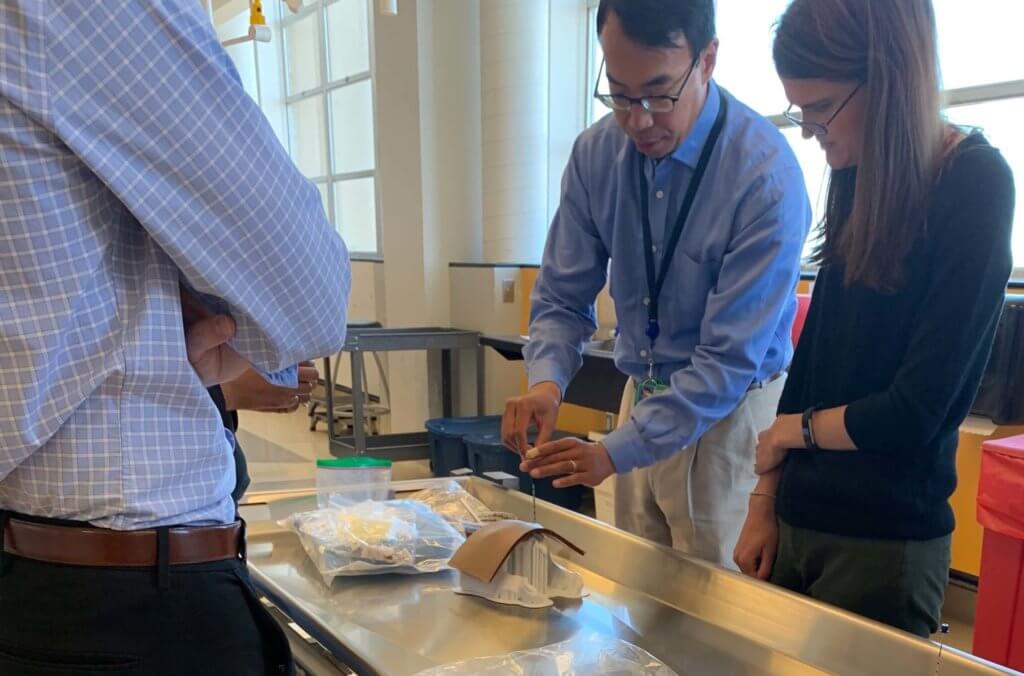
“It went fantastic! The fellows seemed super enthused and we had one third year fellow who went to brush up and was very positive about the experience.”
– Dr. Gerald Hsu, following the simulation.
For future projects, the Department of Hematology and Oncology envisions the simulation models being modified to represent a wide variety of patients, such as layering thicker silicone for bariatric patients or thinning out walls of the 3D model to help simulate elderly patients with osteoporosis. The best part about the 3D modeling process is that the simulation model can be customized in an infinite number of ways and tailored specifically to represent any patient.
The Makers Lab is proud to have collaborated with the Department of Hematology and Oncology and the Anatomy Learning Center in furthering simulation-based learning at UCSF, and we hope to continue fostering interdisciplinary collaboration within the UCSF community. This project was both a great learning opportunity for us and a real journey into the iterative design process.
Do have an idea for a health science simulation project at UCSF? Contact the Makers Lab to get started.

Many thanks to Wes Cayabyab, Simulation Technician at the Kanbar Center, for organizing the silicone suture pad workshops, and to Stacey Yu, Anatomy Lab Manager, for preparing the cadaver lab for the simulation.