This month’s makers are Michelle Nguyen D3, Ashley Wang D3, and Tiffany Yu D3, students in the UCSF School of Dentistry. We caught up with the team to see what they have been making in the Makers Lab.
Q: What did you create?
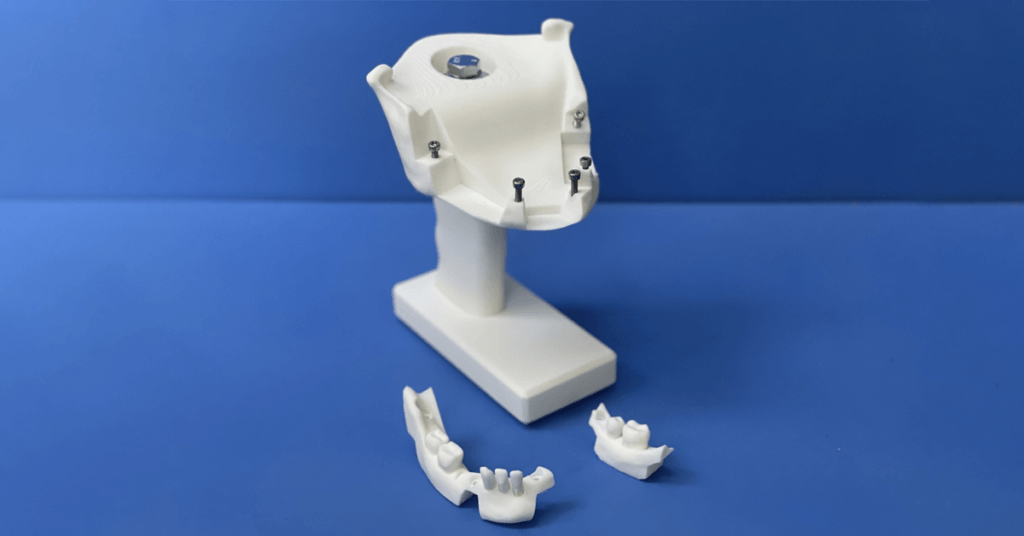
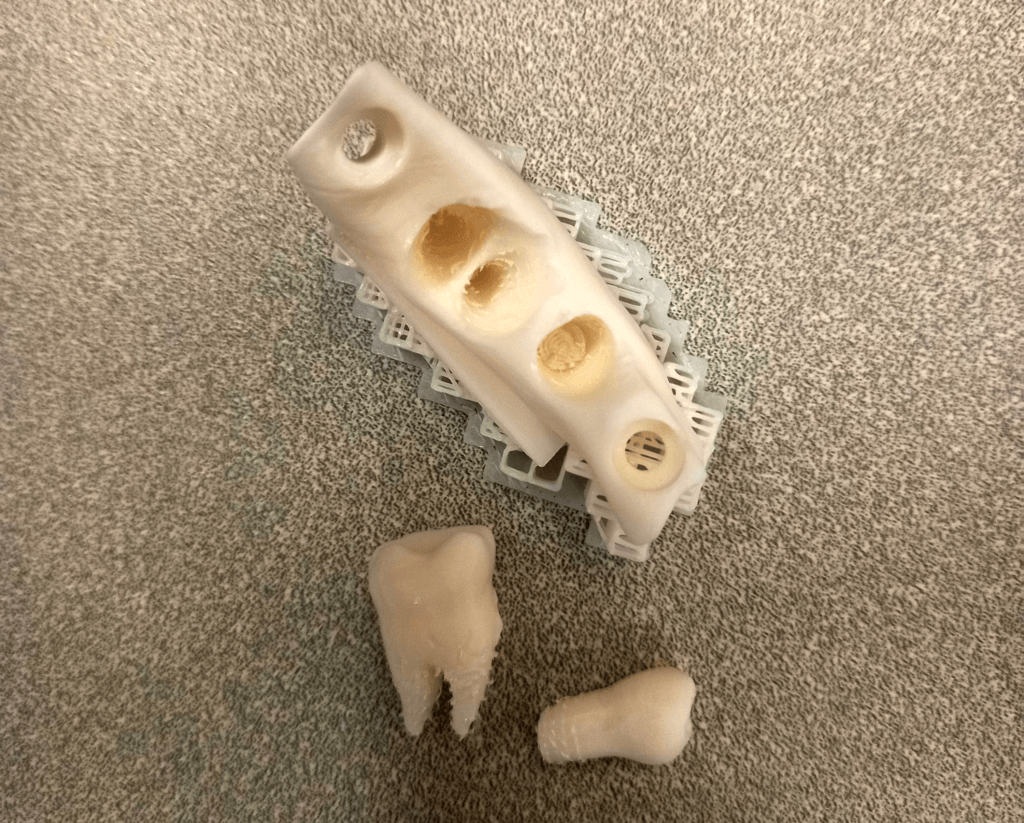
For the Advanced 3D Printing for Health Science Students elective we created a 3D printed mandible that simulates the anchorage of natural teeth to the jaw, via 3D printed “periodontal ligaments.” Calibration of this feature with experienced dentists allowed us to improve the model. Hence, it is similar to natural tooth extraction and assesses the model’s effectiveness for teaching dental students and increasing their confidence in simple extraction procedures before transitioning to patient care. The mandible is printed in several pieces, the main body being a reusable jaw with a handle grip to allow some force to be more safely used during extraction, and several replaceable teeth blocks with the printed “periodontal ligaments” that must be broken to extract the teeth. The design of the handle grip can also be clamped to a solid surface for hands-free use of the simulator.

Q: Why did you decide to create it?
Dental simulation lab experiences are critical for students to learn correct procedural steps, practice techniques with different instruments and materials, and build confidence before transitioning into the clinic. While dental schools excel in providing helpful preclinical experiences in operative, crown and bridge, prosthodontic, and endodontic procedures, there is currently a lack of dental extraction simulation experiences in the dental curriculum prior to performing the procedure on patients. While tooth extraction typodonts are available on the market, little is known about how well they simulate the tactile experience of natural tooth extraction. Our goal was to create something that could fulfill the role of preclinical extraction simulation for dental students.
Q: What was your process like?
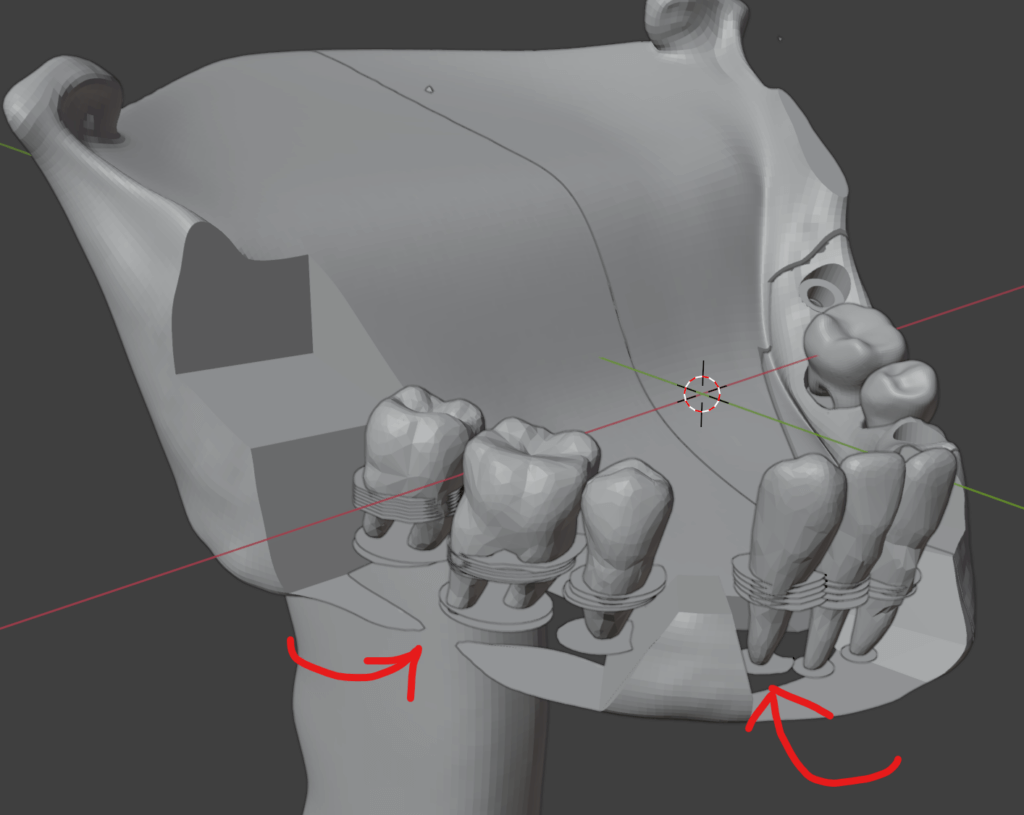
We started with an open-source teeth model and a mandible model from Thingiverse. Using Blender, free and open-source software for 3D modeling and rendering, we modified the tooth STLs to fit our chosen mandible, created socket spaces around the teeth and tried different versions of our artificial periodontal ligaments. From there, we added a handle grip component to the mandible. Then, we sectioned the pieces into the reusable mandible-holder component and the replaceable tooth block components. Finally, we adjusted the prints’ densities before printing them on the Bambu X1 Carbon.
Q: What was the most challenging part of the process?
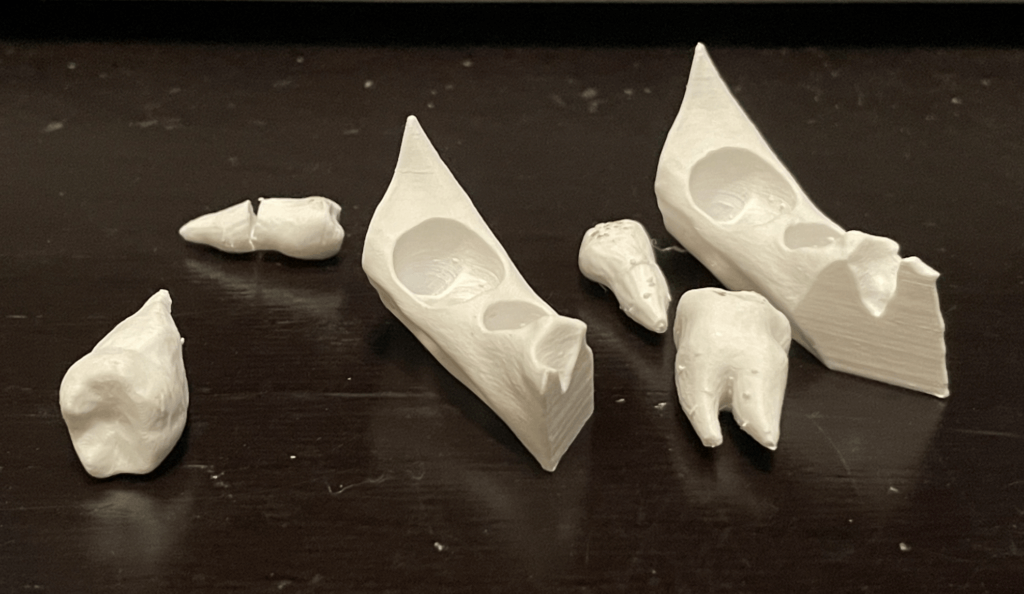
The most challenging part was designing the “periodontal ligaments” and surrounding “bone” to have a tactile sensation and strength as similar as possible to real teeth extractions. The designs required multiple tests with over 25 prototypes and meetings with our periodontist mentor, Dr. Yeh, to narrow down the best designs for our model.
Q: What was your favorite part of the process?
Our favorite part of the process was testing out each prototype until we arrived at our final design. It was exciting to watch our progression from early models, where simulated teeth were overly retentive no matter how much force was used, to models where the teeth would fracture too easily, to our current iteration where the teeth can be extracted predictably with appropriate use of dental extraction instruments.

Q: How has this project contributed to your education?
In seeking advice for improving our model, we also enhanced our understanding of the steps in dental extraction and the purposes of the various tools available for extractions. 3D printing is also becoming increasingly popular in dentistry, so it was helpful for us to learn about various programs used in 3D printing and how to set up a print properly.
Q: What do you plan to create next?
It would be interesting to see if fake gingiva could be added to our model, as the first step in the extraction process involves separating the gingival tissue from the teeth. Following this, it could also be possible to modify the design to include an edentulous space for implant placement practice, where students first open a flap in the fake gums before drilling into the jawbone.