This month’s makers are Zuivanna Rivas MS2, Kamel Awayda MSTP2, and Woodger Faugas MS2, with the UCSF School of Medicine. We caught up with the team to see what they have been making in the Makers Lab.
Q: What did you make?
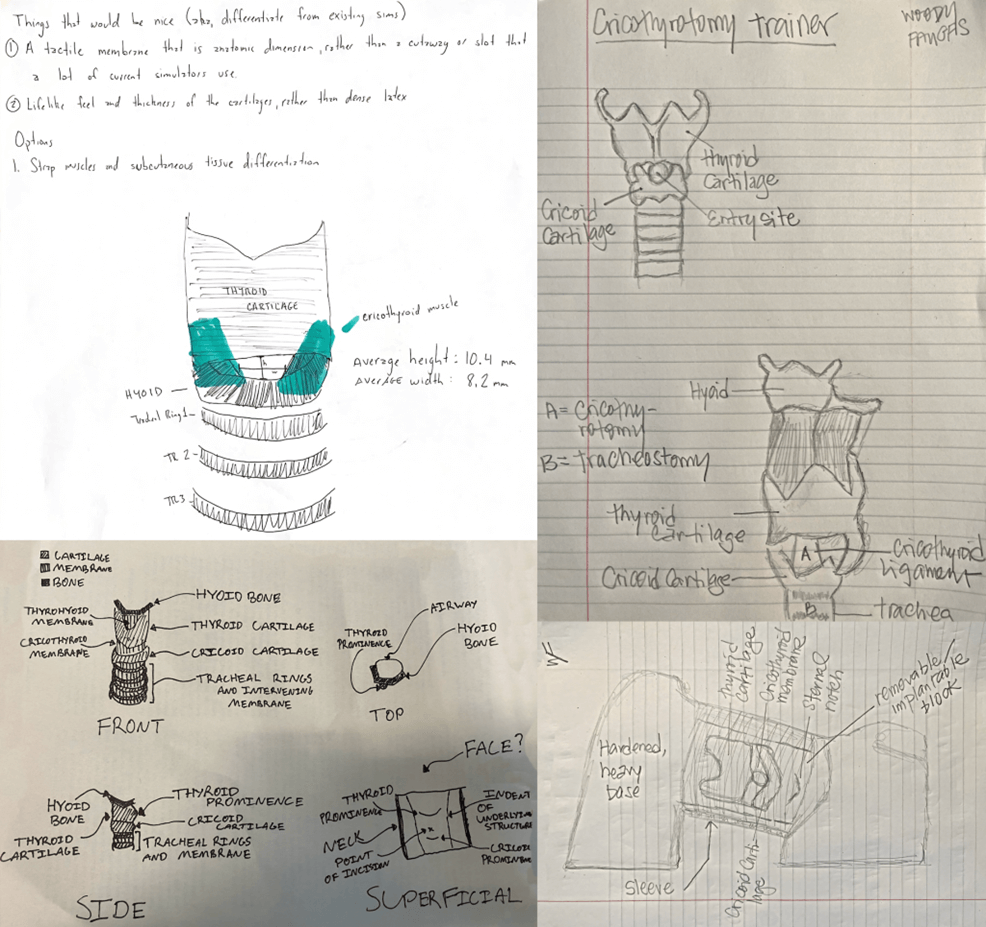
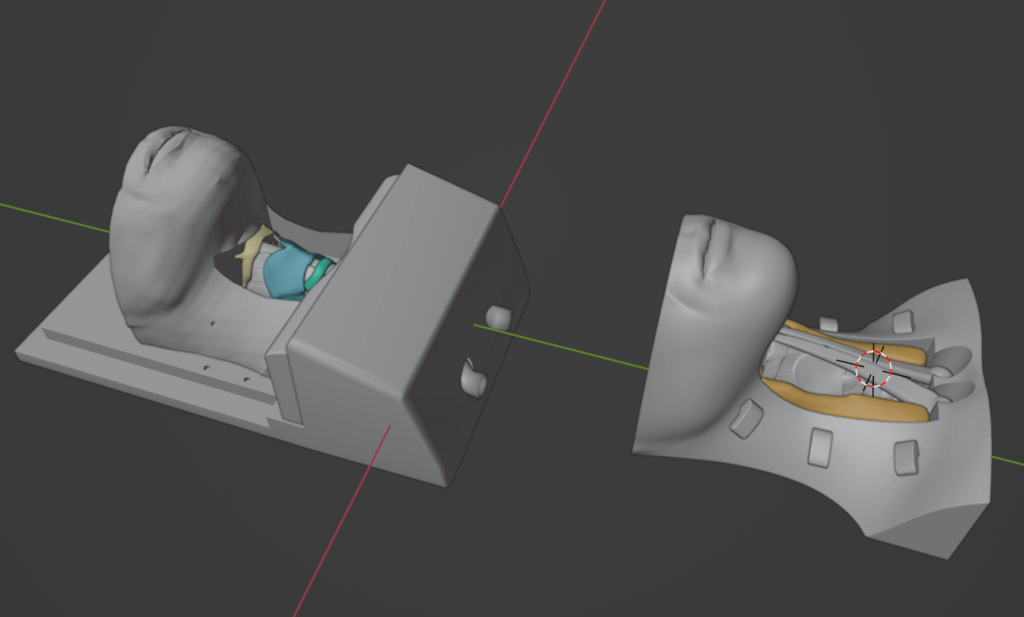
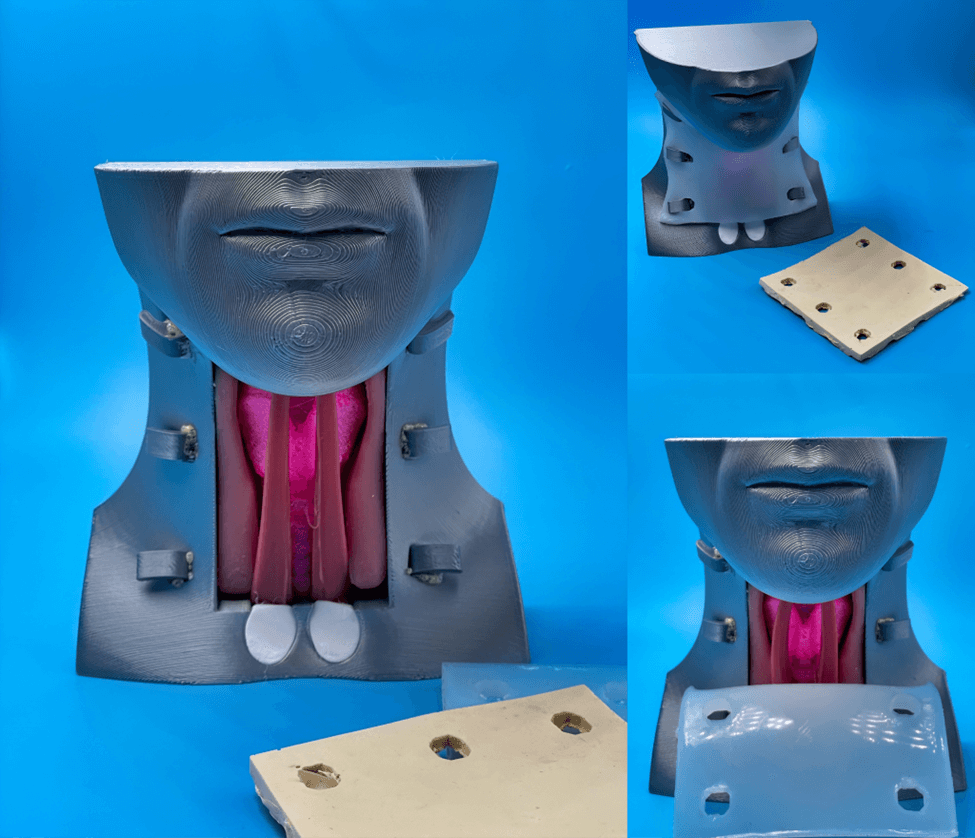
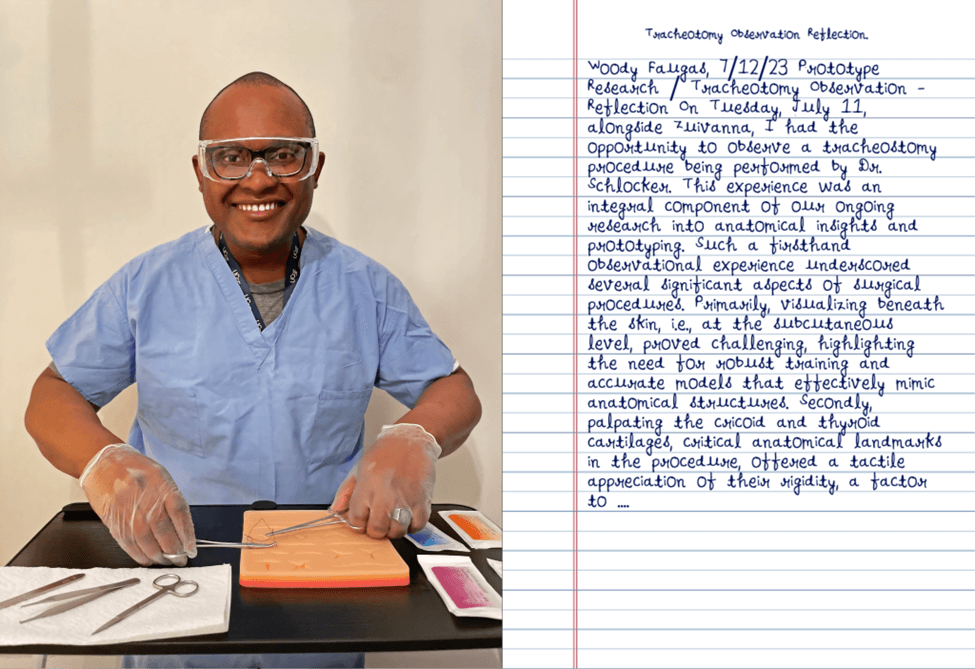
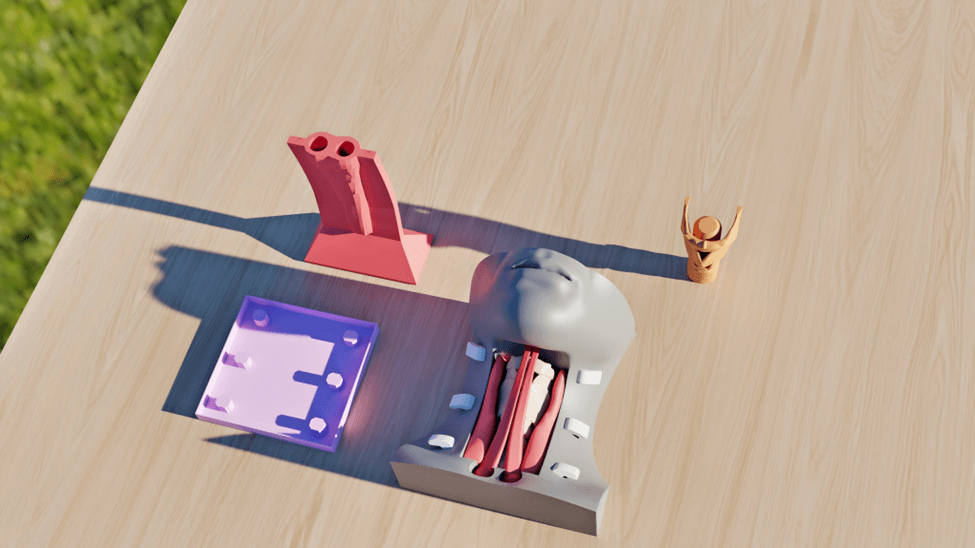
During the Advanced 3D Printing for Health Science Students elective, as well as beyond, our collaborative team, namely Woodger G. Faugas (or Woody Faugas), Kamel Awayda, and Zuivanna Rivas, embarked on the creation of a 3D printed, high-fidelity cricothyrotomy (HFC) trainer (or simply CT, for “Cric. trainer”). This groundbreaking project was conducted in collaboration with Otolaryngologist Caroline M. Schlocker, MD, designer Scott Drapeau, MA, and Assistant Anatomy Professor Madeleine Norris, PhD, MSc, with invaluable support from Makers Lab Manager Dylan Romero, MA. 3D printing and engineering roles in this endeavor were well-defined. And in this vein, Woody served as the team leader, developing and monitoring the overall collaboration, engineering, design, and prototyping strategies, coordinating recurring meetings, and taking the lead in the technical and surgico-anatomical aspects of developing and refining our model, e.g., in Blender. Kamel also actively participated in software-based model development and conducted materials research, whereas Zuivanna focused on design and materials research.
At its core, this medical technology (MedTech) project entailed interpreting and accessing medical imaging studies, e.g., CT scans and X-rays, as well as generating 3D criteria-concordant models from Digital Imaging and Communications in Medicine (DICOM) data (e.g., CT, MRI) using segmentation. Extensive research and reading also transpired, to review, catalog, present, and discuss a large amount of existing literature, alongside best practices in pertinent fields (e.g., Otolaryngology, Emergency Medicine, and even Dermatology). Such a collaborative, months-long, and cross-disciplinary effort resulted in the creation of an HFC trainer that addresses a genuine, outcome-determinative need for more anatomically accurate and cost-effective cricothyrotomy simulation (CS) models. In moving forward, it’s worth noting that whereas all HFC trainers and CS models are, or encompass, CTs, not all CTs are high-fidelity and not all CS include HFC trainers, with this varied terminology reflecting the diversity of capacity in Cric. trainers used.
Q: Why did you decide to create it?
The decision to create our 3D-printed HFC trainer was driven by the recognition of a significant gap in the educational value or accessibility of presently available CS models. With cricothyrotomy being synonymous with cricothyroidotomy, current cricothyroidotomy simulation models are either prohibitively expensive or lack anatomical accuracy, furnishing learners (e.g., medical students and residents) with unreachable or misguiding, and thus unfruitful, experiences. The primary objectives of our project entail(ed) improving current simulation techniques, rapid prototyping with 3D printing technology, incorporating expert opinions in developing an anatomically accurate simulator, and making emergency cricothyroidotomy simulation accessible, accurate, cost-effective, and reproducible.
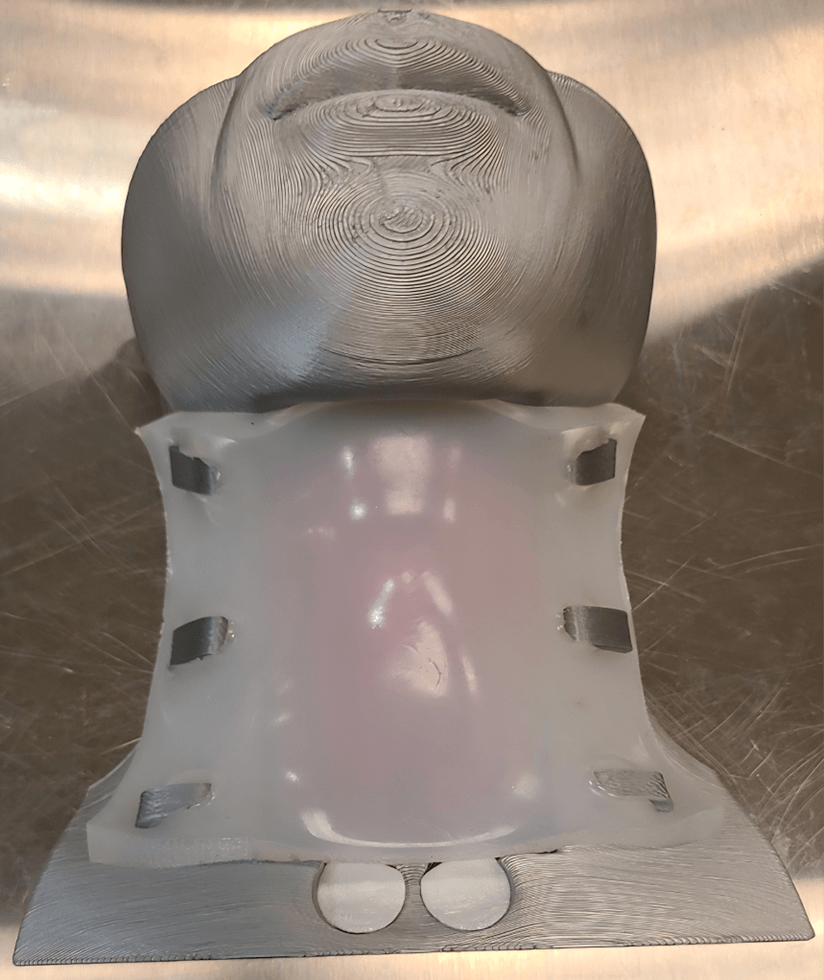
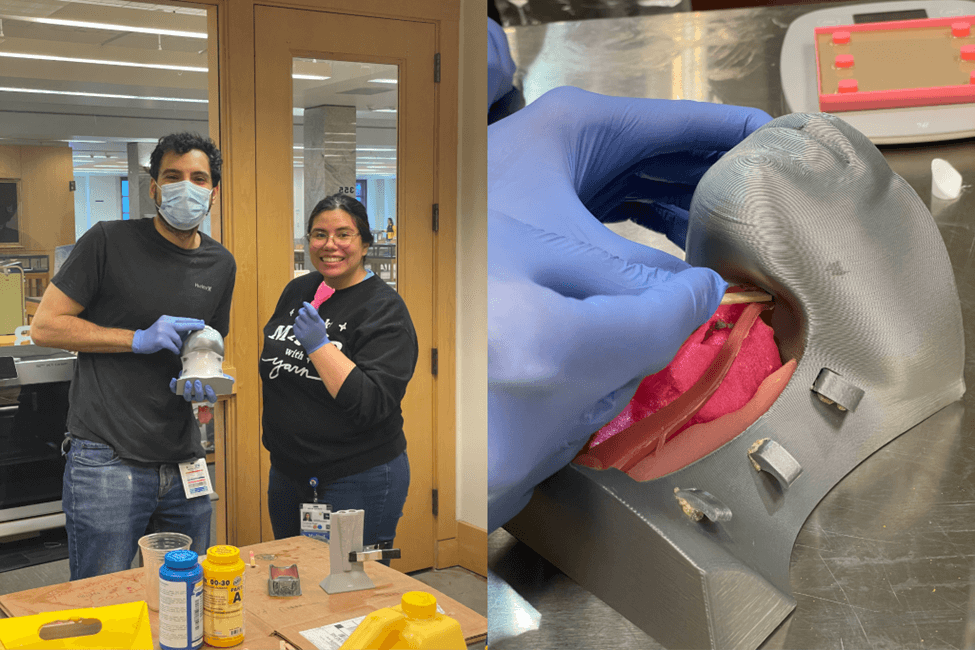
Methodologically, our work involved using 3D-modeling software, a desktop 3D printer, and anatomical data to create an accurate model of involved cartilaginous structures (e.g., cricothyroid cartilage). We also researched and analyzed proper wound care, post-surgical scar management, and scar tissue reduction (e.g., via dermabrasion, chemical peels, and injections). Our model drew from dimensions procured via anatomical studies and measurements realized at the UCSF Anatomy Learning Center, our institutional donor lab. Multiple iterations were made, guided by feedback from all of the team — especially designer Scott Drapeau, Dr. Schlocker, and Dr. Norris, to ensure anatomical accuracy. The result of our interdisciplinary collaboration is a low-cost (~$12), anatomically accurate model that can be assembled with a membrane and skin for enhanced realism. Such an innovative design provides a highly realistic simulation for practicing critical skills in airway surgery, including landmarking, incision, and intubation.
Q: What was your process like?
Our collaborative process was both longitudinal and multidisciplinary —involving team members from intersecting backgrounds and expertise areas. We worked together over an extended period while managing our rigorous, cotemporaneous academic, research, and service commitments. The process encompassed several key elements: technical skills application and refinement in Blender, a 3D modeling software, collaboration, prototyping, expertise in Blender features, proficiency in some areas of cervical anatomy, attention to detail, on top of meticulous planning. This journey required independent engineering, effective communication, alongside continuous improvement. It demanded an understanding of both the medical aspects and the technical intricacies involved in creating an anatomically accurate model.
Q: What was the most challenging part of the process?
The most challenging aspect of our project entailed creating something for which there was no existing model or clear template. Given the lack of pre-existing 3D models, we needed to develop a highly accurate and cost-effective HFC trainer from scratch. In our pursuit of solutions and given the breadth and depth of work involved in model development, we initially explored using Python scripting within Blender to automate repetitive subtasks. However, we quickly encountered challenges with the unsatisfactory results produced by these scripts. Blender, as a powerful open-source 3D software, can be extended using Python. While Python scripting offered potential scalability and prototype iteration benefits, it did not align with our goals of achieving, inter alia, anatomical accuracy, cost-effectiveness, accessibility, and reproducibility. Our focus shifted towards granular model development and editing, which allowed us to have greater control over the intricacies of the trainer. Each constitutive organ of our model was meticulously created using mesh objects, a process requiring precision and attention to anatomical details. Overcoming these challenges undoubtedly required drawing upon our team’s dedication and problem-solving abilities.
Q: What was your favorite part of the process?
One of the most rewarding aspects of this project encompassed the opportunity to acquire new skills and expertise. Our experience with Blender, in particular, proved enriching. In learning about a plethora of applications, as part of completing this project, we discovered the full potential of Blender’s capabilities. Furthermore, solving this vital need in various domains of medicine enabled us to bridge our design and software engineering skills with our anatomical knowledge. This interdisciplinary approach proved intellectually and indelibly stimulating, allowing us to assess and develop hypotheses anent real-world applications of our diverse skill sets. The process of learning, innovating, and applying our knowledge to newly create a technology-formulated training apparatus with a profound impact on patient care, medical education, multiple medical subspecialties (e.g., Otolaryngology, Emergency Medicine, Dermatology, and surgical medicine) is undeniably gratifying. In many ways, it serves as a reminder of the importance of continuous learning and collaboration in the pursuit of meaningful and care-improving projects.
Q: How has this project contributed to your education?
This advanced 3D printing project has made significant contributions to our education in several, key ways. First, we deepened our understanding of human anatomy, particularly in the context of the cervical region, as well as Otolaryngology/Head and Neck Surgery, Emergency Medicine, Dermatology, Plastic Surgery, among others. Creating an anatomically accurate CT necessitated a comprehensive grasp of the relevant anatomical structures. Second, our proficiency with Blender and 3D modeling software improved substantially. We gained hands-on experience in utilizing these tools for medical applications. Third, the project fostered a spirit of humble inquiry as we delved into research, brainstorming, planning, designing, and prototype revision. This inquisitive mindset was crucial to the project’s success. Lastly, and crucially, our involvement in this project nurtured our interests in innovation and medical technology (MedTech). We realized the potential for 3D printing, and adjacent technolog(y/ies), to revolutionize medical education and training through facilitating hands-on spaced repetition. Woodger, in particular, had the opportunity to learn about and practice suturing, a valuable skill in understanding skin thickness and its implications for cricothyrotomies, primarily, and scar healing, secondarily. Additionally, we gained exposure to head and neck surgeries, thanks to Dr. Schlocker’s precepting, mentorship, and other supportive contributions. This exposure provided fundamental surgical education information that enhanced our overall medical knowledge.
Q: What do you plan to create next?
Looking ahead, our plans will consist of building upon the foundation we’ve established with the HFC trainer or CT. Our goals for the future, therefore, will include creating additional prototypes of our model — with a focus on further refinement and enhancement. We also aim to explore the possibility of deriving protectable intellectual property rights related to our model, making it available to the public for free non-commercial use, with commercial use rights potentially excluded. Additionally, we plan to work towards publishing one, or more, research article(s) documenting our work, methodology, and findings — sharing our insights with the health sciences, in addition to medico-surgical and educational communities. Each of us intends to pursue individual projects in alignment with our respective medical fields of interest. These projects will contribute to our continued epistemic growth and specialization. In closing, the creation of this 3D-printed HFC trainer constitutes an important achievement, made possible through multi-level faculty guidance, multidisciplinary collaboration, innovation, and a commitment to improving patient care and medical education. Our future endeavors will build upon this foundation as we strive to make meaningful contributions to the field of medicine.
Acknowledgements
This project was made possible by a 2023 Innovations Funding for Education grant from the UCSF Academy of Medical Educators Innovations Funding Program.
