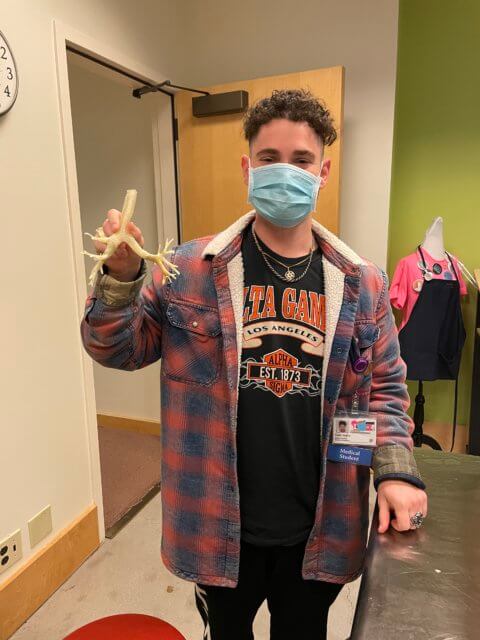
This month’s maker is Samuel Vydro, MS3, UCSF School of Medicine. We’ve had the pleasure of working with Sam since last year’s Advanced 3D Printing for Health Science Students elective. We caught up with Sam to see what he made.
Q: What did you make?
The team and I made a 3D printed tracheobronchial model that we hope will be used for pulmonology bronchoscopy training here at UCSF!

Q: Why did you want to make it?
At first, I came into contact with Dr. Christopher Leba through UCSF’s advanced 3D printing elective and he pitched this project. As I went through all the trials and tribulations that came with learning the software, I became really invested in making our model. The thought to use such an array of imaging and engineering modalities to create something that could be used for training at such a prestigious institution was really exciting to me, so I wanted to dedicate as much time as I could.
Q: What was your process?
Well, I started with a lot of reading. 3D printing was new to me, so I had to learn a lot of the prior work that’s been done in both the pulmonology sphere and 3D modeling as a whole. The software to create real life anatomic models from CT scans was fascinating to me, but I had to watch a lot of YouTube videos and read a lot of articles on how to get the hang of it. After I had the base model rendered, the process was essentially having a bunch of meetings with my biggest partner – Scott Drapeau from the Makers Lab.
Through tireless hours of work, we were ready to print and from there, it was time for good ol’ arts and crafts. We glued, we painted, we sculpted, we encased bronchi in silicone. Going into too much detail would turn this into a paper, which I do hope to write up after we’re all done.


Q: What was the hardest part of the process?
The hardest part of the process was most definitely going through the trial and error of building the first model. Specifically, getting all our dissolvable PVA out of the bronchial tree. There were A LOT of nooks, crannies, twists, and turns which made it super difficult to fish all the PVA out. And as you can imagine, if the inside of the model is not hollow, it’s not very useful for bronchoscopy training. It led to a lot of headaches for Scott and me, but we were really happy with the first product and look forward to Prototype 2.0 being even better.
Q: What was your favorite part of the process?
I know I just said that building had many, many, many challenges, but it was also super fun. All the obscure problem-solving Scott and I were able to think up really made me feel like I was some sort of medical, 3D printing MacGyver. So, despite the headaches, it was definitely my favorite part of the process.

Q: How did this help make you a better student?
Right now, I am just a medical student that isn’t completely sure what I want to do for the rest of my life, but I am currently interested in pursuing a career in radiology. I think all the work I did with generating the model from CT scans via DICOM files made me more aware of how imaging can be used in creative ways. 3D printing definitely opened up different avenues to pursue research going forward for me, especially in the realm of creating cost-effective models for training and teaching. Maybe one day, I can do some work on building affordable medical equipment for lower funded regions and hospitals.
Q: What do you want to make next?
This is the hardest question yet, and I have a lot of ideas. The first thing that came to mind was building some sort of large arterial tree with real clinical fidelity that could be used in Interventional Radiology to help get residents accustomed to maneuvering various wires and catheters in different clinical situations before getting real exposure in the IR suite.

