This week’s maker is Crystal Zhou, PharmD, APh, AHSCP, BCACP, assistant clinical professor in the UCSF School of Pharmacy. We caught up with Dr. Zhou in between classes to see what she has been making in the Makers Lab.

Q: What did you make?
The School of Pharmacy partnered with the UCSF Makers Lab to create 3D models of the GI tract (from esophagus to rectum) and liver.

Q: Why did you want to make it?
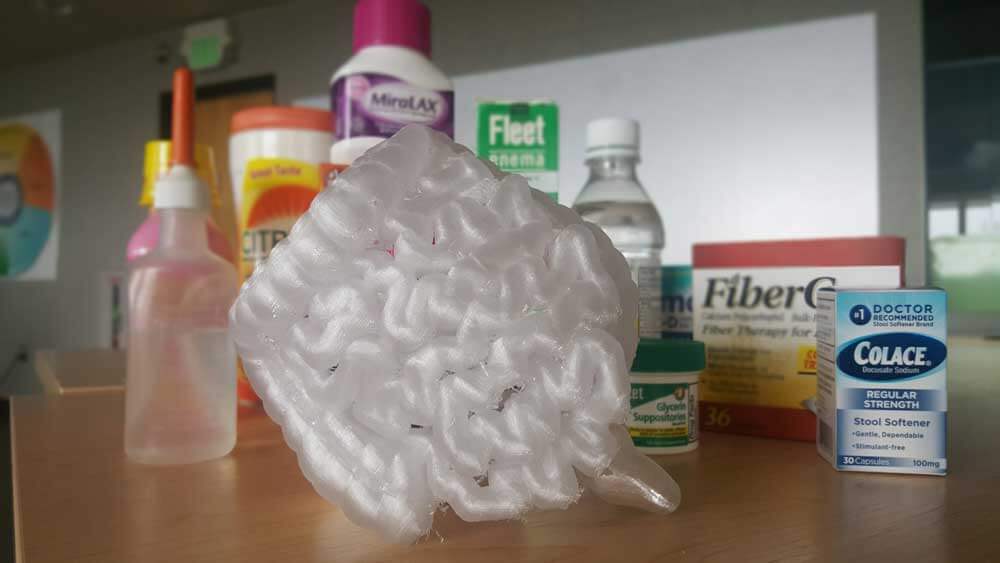
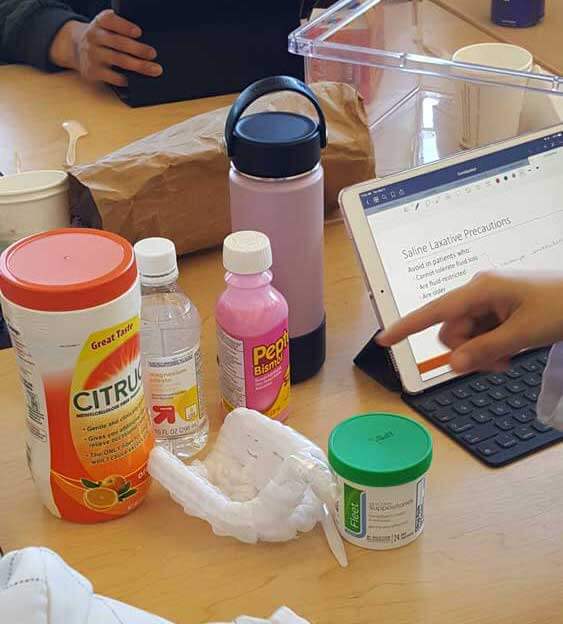
The Applied Patient Care Skills (APCS) course is a new, hands-on course that is part of the School of Pharmacy 3-year competency based curriculum. The APCS course focuses on hands-on skills, patient communication skills, and problem-solving and critical thinking skills. The 3D GI tract models were made to help with the patient counseling aspect of rectal formulations of medications. We did not quite have a way to teach students about rectal formulations (enemas, suppositories), which are also hard to counsel patients on if you have never seen or used them. Therefore, the 3D models that were created allowed the students to practice rectal administration of medications and also practice counseling patients on “how-to” administer these medications.
Q: What was your process?
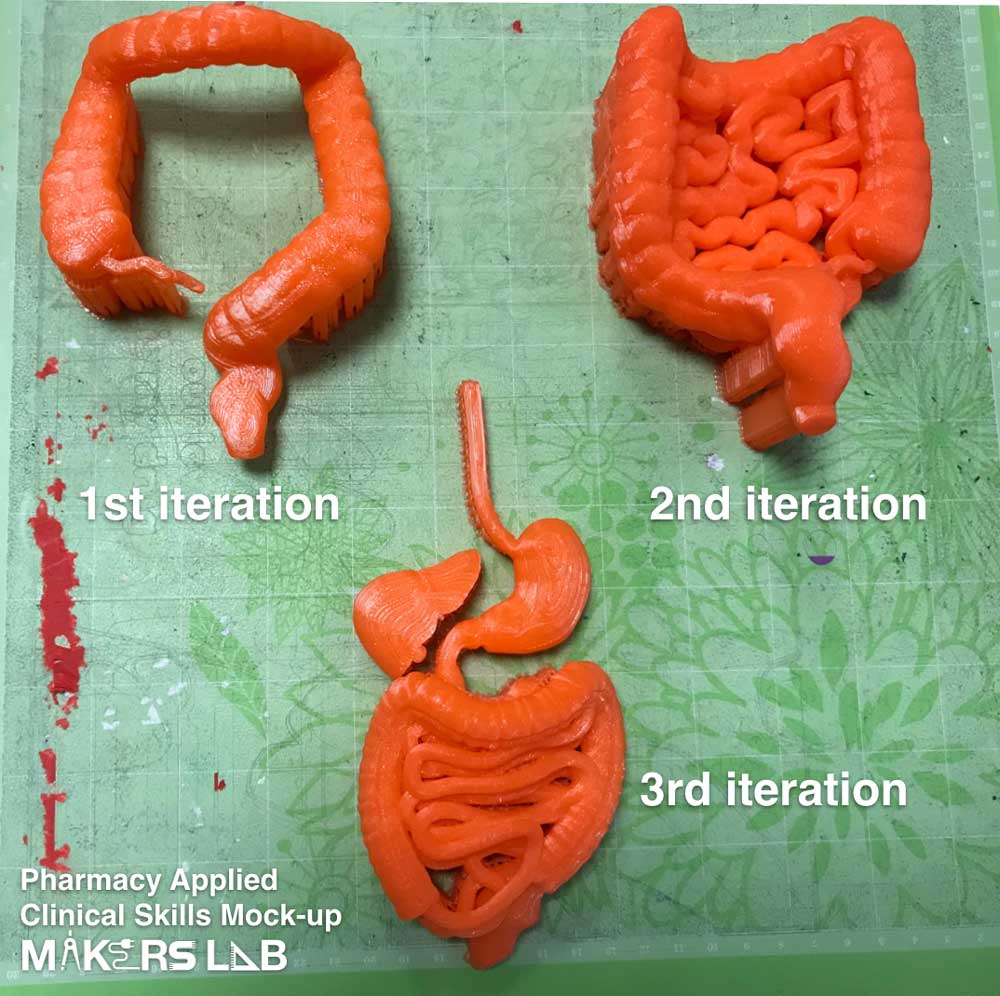
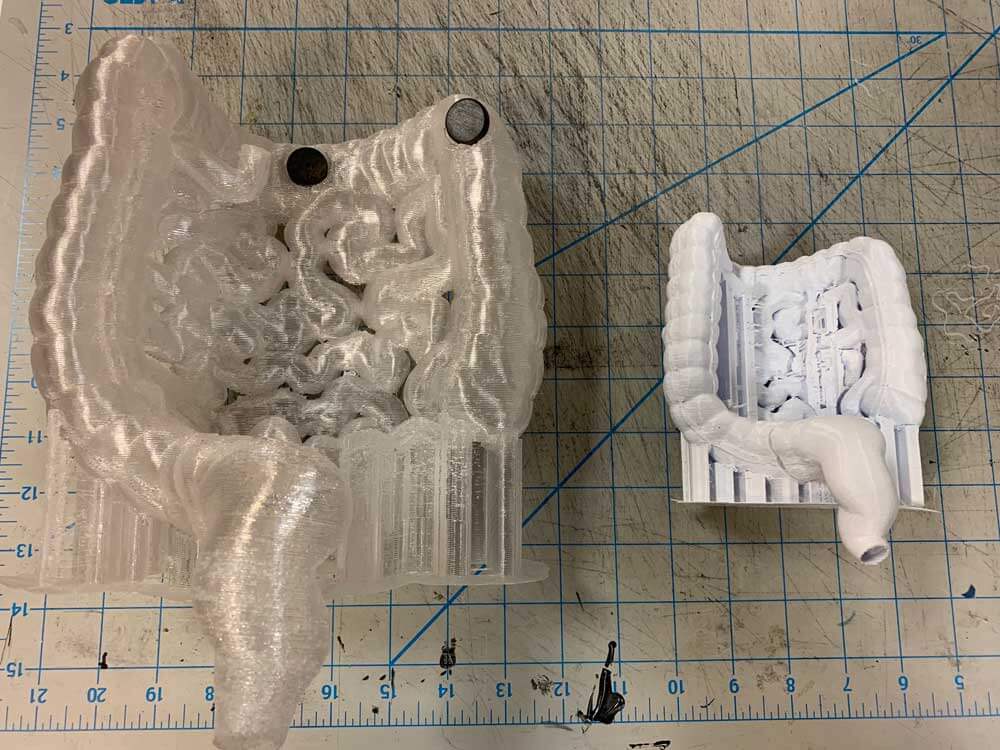
There were multiple iterations of the project. We used multiple 3D models from the NIH 3D Exchange and Thingiverse and modified them so we could connect each part with magnets. We met with Makers Lab staff after each iteration of the model was completed to provide feedback on the model and make it more useful for the purpose of the course. We completed 4 versions of this model until we created a final version for use in the classroom.
Q: What was the hardest part of the process?
The hardest part of the process was imagining what we wanted that could be usable in the classroom. Luckily, Dylan was able to capture my words and created exactly what I had described and turned it into a usable model!
Q: What was your favorite part of the process?
My favorite part of the process was re-working each of the previous models. I feel like every time we met to talk about how to improve the model, it became even better and made me more excited to teach using these models in the classroom.
Q: Why did you make it instead of buying it?
We decided to make these models so that we could customize them for our purpose. I couldn’t find any models online that had a hollow rectum for the students to practice using and counseling on enemas. Making the models also allowed us to customize the size of the model, which is very important.
Q: How did this help make you a better educator?
I am a strong believer that if students are able to touch and feel the medication products based on first-hand experience, they are more likely to be successful later on because of this experience. With these models, I was able to make that happen for our students.
Q: What do you want to make next?
I want to continue making different organ system models that will allow our students to have more hands-on practice with medication administration. One thing that I have been thinking about is a model of the kidneys that we can adjust the creatinine clearance for!